Safety Tips: Preventing Frostbite and Hypothermia
Prolonged exposure to low temperatures, wind or moisture-whether it be on a ski slope or in a stranded car-can result in cold-related illnesses such as frostbite and hypothermia. The National Safety Council offers these tips to help you spot and put a halt to these winter hazards.
How to detect and treat cold-related illnesses
Frostbite is the most common injury resulting from exposure to severe cold. Superficial
frostbite is characterized by white, waxy, or grayish-yellow patches on the affected areas. The skin feels cold and numb. The skin surface feels stiff but underlying tissue feels soft and pliable when depressed. Treat superficial frostbite by taking the victim inside immediately. Remove any constrictive clothing items that could impair circulation. If you notice signs of frostbite, immediately seek medical attention. Place dry, sterile gauze between toes and fingers to absorb moisture and to keep them from sticking together. Slightly elevate the affected part to reduce pain and swelling. If you are more than one hour from a medical facility and you have warm water, place the frostbitten part in the water (102 to 106 degrees Fahrenheit). If you do not have a thermometer, test the water first to see if it is warm, not hot. Rewarming usually takes 20 to 40 minutes or until tissues soften.
Deep frostbite usually affects the feet or hands and is characterized by waxy, pale, solid skin. Blisters may appear. Treat deep frostbite by moving the victim indoors and immediately seek medical attention.
Hypothermia occurs when the body’s temperature drops below 95 degrees Fahrenheit. Symptoms of this condition include change in mental status, uncontrollable shivering, cool abdomen and a low core body temperature. Severe hypothermia may produce rigid muscles, dark and puffy skin, irregular heart and respiratory rates, and unconsciousness. Treat hypothermia by protecting the victim from further heat loss and calling for immediate medical attention. Get the victim out of the cold. Add insulation such as blankets, pillows, towels or newspapers beneath and around the victim. Be sure to cover the victim’s head. Replace wet clothing with dry clothing. Handle the victim gently because rough handling can cause cardiac arrest. Keep the victim in a horizontal (flat) position. Give artificial respiration or CPR (if you are trained) as necessary.
How to prevent cold-related illnesses
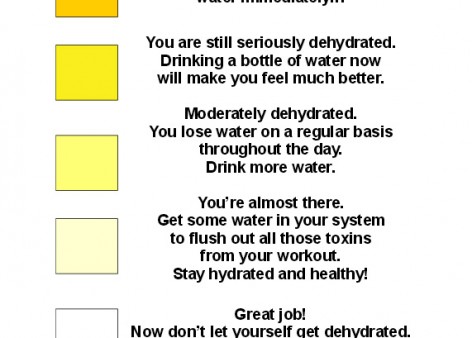
Avoid frostbite and hypothermia when you are exposed to cold temperatures by wearing layered clothing, eating a well-balanced diet, and drinking warm, non-alcoholic, caffeine-free liquids to maintain fluid levels. Avoid becoming wet, as wet clothing loses 90 percent of its insulating value.
View these tips as a PDF